INSANE: How COVID hurt the fight against other dangerous diseases – My Comments
[Check this out, especially the chart of measles near the bottom. By focusing on this COVID crap, this is actually harming the fight against other diseases that are real and dangerous! Nature is one of the top scientific journals in the world. So this is a weird twist to this COVID crap that I had never expected. Jan]
After India went into lockdown in March 2020, the number of new tuberculosis (TB) cases detected there each day dropped by an alarming 70% in one month. “It freaked us out,” says Lucica Ditiu, executive director of the Stop TB Partnership, an organization in Geneva, Switzerland, that was set up to help combat TB, a disease that kills 1.4 million people a year.
Ditiu was worried because the fall in India, the only country that collects real-time TB data, showed that cases were going undiagnosed and untreated as many nations diverted medical resources to tackling COVID-19. TB transmission would increase, she knew, because the disease is generally passed on through close contacts (at home or in prisons, for instance), which social distancing would be unlikely to prevent. And increased transmission would lead to more deaths.
Her fears were borne out. This March, the World Health Organization (WHO) announced that the number of people receiving TB treatment globally had dropped by more than one million, setting the fight against the disease back by a decade or more. An estimated 500,000 more people than usual might have died of TB last year, the WHO said.
“We face a potential calamity,” said Peter Sands, executive director of the Global Fund to Fight AIDS, Tuberculosis and Malaria, at a Stop TB Partnership press briefing.
The COVID-19 pandemic has disrupted prevention and treatment of a host of diseases. As countries went into lockdown last year, mass vaccination campaigns for measles, polio, meningitis and more ground to a halt, leaving millions of children at increased risk of deadly, preventable diseases. Some health facilities were closed; health-care workers were redeployed to fight the pandemic. Shipments of essential medicines and devices were delayed, and fewer people than usual sought treatment at clinics for fear of catching COVID-19.
Three million COVID deaths is a grim milestone
More than a year into the pandemic, analysts are trying to gauge its impact on diseases that have largely slipped from public attention. For many diseases, it is too soon to see direct increases in illness and deaths, so researchers must rely on indirect measures — such as the number of children who have not been vaccinated, or falls in diagnoses — or on models, which are imperfect tools at best. Together, the data suggest that the knock-on effects of the pandemic could be larger than those caused by COVID-19 itself — and that they will linger long after the pandemic has ended.
The ramifications can be seen all over the globe, but the greatest effects will be felt in some of the poorest, most vulnerable countries, where health systems are already fragile. Three diseases typify COVID-19’s worrying impacts: TB, the biggest killer among all infectious diseases, especially among poor and marginalized people; measles, one of the most contagious viruses known, which is a major killer of young children in poor countries; and polio, the only virus currently targeted for eradication, which is clinging on in some parts of the world.
Tuberculosis time bomb
Last year, COVID-19 overtook TB as the infectious disease that caused the most deaths globally, but in low- and middle-income countries, TB was still the biggest killer. Caused by a bacterium (Mycobacterium tuberculosis), TB eats away at the lungs and kills its victims slowly, often years after the onset of an active infection. About 2 billion people worldwide have latent TB infections in which their immune systems control the bacteria; 5–10% of those individuals will develop active TB in their lifetime. The 100-year-old bacillus Calmette–Guérin (BCG) vaccine can halt progression to severe forms of TB in children, but it does not prevent infection.
To tackle TB, physicians need to diagnose it and then treat it with a gruelling six-month regimen of medicines that can stretch to two years for drug-resistant strains. So Ditiu started to worry last March when she heard from other pulmonary specialists in her native Romania and elsewhere that they were being pulled away from TB to care for people with COVID-19. Some TB hospitals, well practised in dealing with a contagious respiratory disease, were being repurposed. During lockdowns, people with TB were having a hard time getting to clinics for diagnosis or to pick up their drugs. Then the India figures showed diagnoses plummeting.
The Stop TB Partnership soon teamed up with Imperial College London and others to model the impact of COVID-19 on the TB burden. In their worst-case scenario, released last May, a 3-month lockdown with a 10-month recovery to normal TB services would lead to 6.3 million additional cases and 1.4 million excess TB deaths worldwide between 2020 and 2025 (see go.nature.com/3dtjx7t).
Last year’s worst-case scenario now seems too optimistic, says Nimalan Arinaminpathy, a medical epidemiologist at Imperial who co-authored the study. Because TB moves so slowly, it is too soon to know whether more people died of TB than expected last year. But indirect signs of trouble are abundant. This March, the WHO said that, around the world, 21% fewer people received care for TB in 2020 than in 2019, a fall of 1.4 million (see ‘Tuberculosis falling off the radar’). This formed the basis for its estimate that an extra 500,000 people have died of TB. Although India rebounded from its diagnosis nadir with an aggressive TB programme to regain lost ground, the number of newly detected cases there is still about 12% shy of where it was pre-COVID, say Ditiu and Harsh Vardhan, India’s minister of health.
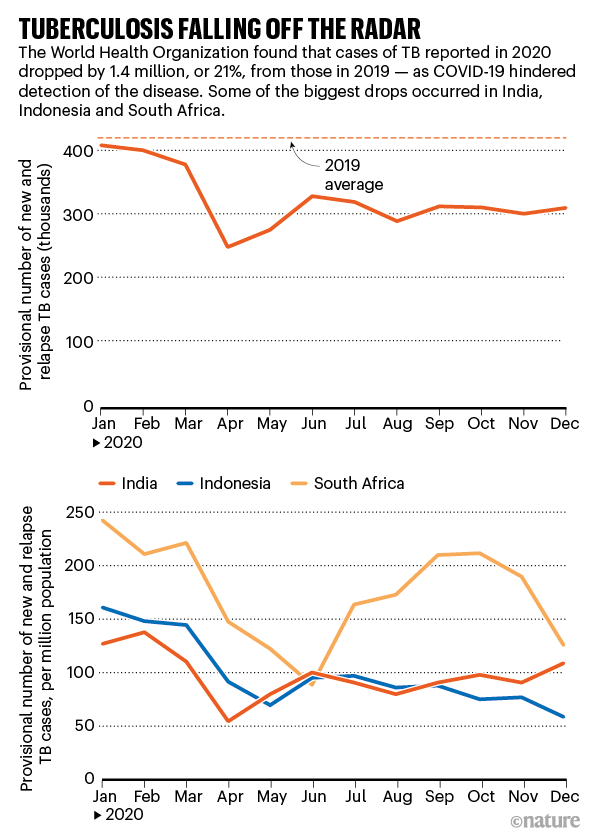
Source: WHO
The worst effects of the pandemic on TB services can be mitigated — with concerted effort and money, says Suvanand Sahu, deputy executive director of the Stop TB Partnership. “Recovery does not happen by default.” In India, the national TB programme has begun giving people with the disease at least a month’s supply of drugs, to avoid them having to make frequent trips to the clinic. Instead of health workers watching patients swallow each dose in person to be sure they stick to the regimen, visits are done by video. Some TB centres are simultaneously testing people for both COVID-19 and TB. And the country is moving towards active case finding — going out into the community to identify infected people, instead of passively waiting for them to seek care.
In an ideal world, all countries would do this and more to fight TB, “but we are talking about countries with public-health systems that are stressed”, says Arinaminpathy.

Medical staff screen people for tuberculosis and leprosy in Mumbai, India. Health workers are increasingly going into communities to identify people with these diseases to combat concerns that cases will be missed because of the pandemic.Credit: Rafiq Maqbool/AP/Shutterstock
Measles menace
Before the coronavirus pandemic hit, global measles cases had soared to nearly 870,000 in 2019, with almost 210,000 deaths, mostly in young children. This was the highest level in decades, largely because underfunded health systems had struggled to keep up with routine childhood immunizations or conduct the large vaccination campaigns they rely on to ward off outbreaks when childhood immunization rates are low. The measles virus is extremely contagious, and can cause diarrhoea, loss of sight or hearing, pneumonia and encephalitis (swelling of the brain). In combination with malnutrition, it kills an estimated 3–6% of those it infects in poor countries.
So it was a blow in March 2020 when the WHO told countries to temporarily suspend all mass vaccination campaigns. By April, many countries had abruptly cancelled or postponed their campaigns. In May, the WHO issued guidance for safely resuming, but 24 countries still have not done so (see ‘Measles vaccinations on hold’). James Goodson, a senior measles scientist at the US Centers for Disease Control and Prevention (CDC) in Atlanta, Georgia, fears that those scheduled for 2021 will slip as well.
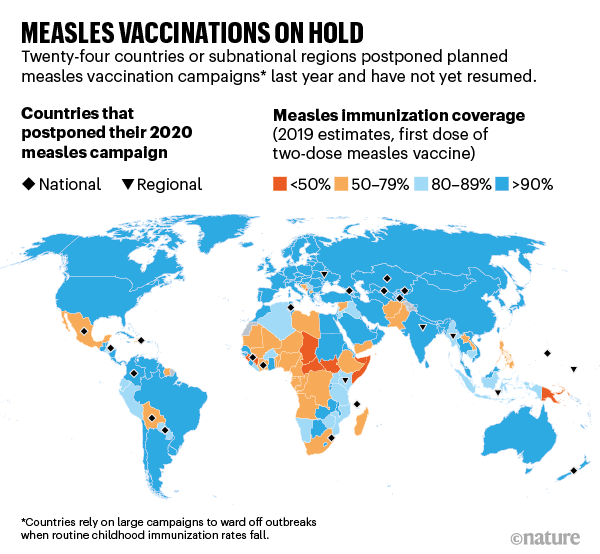
Source: CDC/WHO
For now, global measles cases remain curiously low. In 2020, they were down to about 89,000 (see ‘Measles: rise and fall’). Hampered surveillance might explain part of the drop, and because so many children caught measles in 2019, natural immunity levels are high. But the biggest factor, measles scientists say, is that COVID-19 lockdowns, travel restrictions and physical distancing have reduced the population mixing that fuels the spread of the measles virus. (In the United States, for instance, where the virus is typically brought in by travellers, measles cases fell from almost 1,300 in 2019 to just 13 in 2020.)
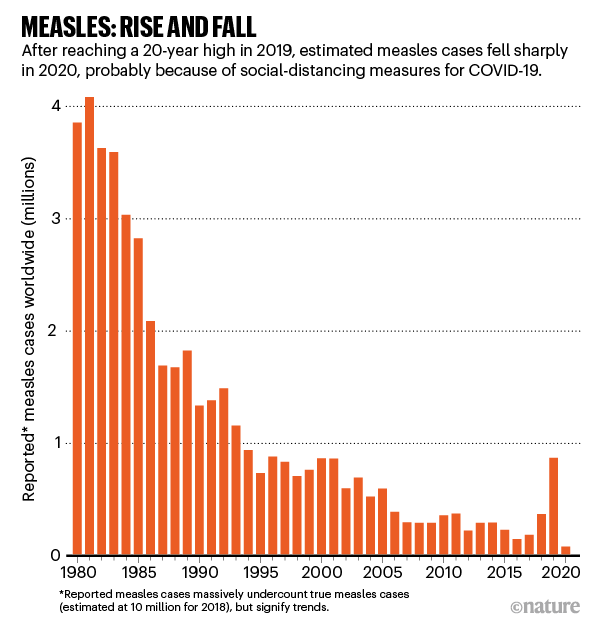
Source: WHO/UNICEF/CDC
Measles experts fear that this is the calm before the storm. The delayed campaigns have left a huge and growing pool of young children susceptible to measles. When the virus finds them, as COVID-19 restrictions ease, it will tear through the unprotected population. “We are sitting on a tinderbox,” says Goodson. He anticipates huge outbreaks this year and next, unless countries act soon.
The 2014–15 Ebola outbreak in West Africa shows what can happen when attention is diverted from measles, says epidemiologist Balcha Masresha at the WHO’s regional office for Africa in Brazzaville, Congo. The outbreak upended health services as workers were sidetracked by Ebola, or died, and as clinics and other facilities shut. The number of children vaccinated against measles monthly fell by roughly 25% in 2014 and 2015 in Liberia and Guinea, two of the worst-affected countries. Although mass campaigns resumed in 2015, Liberia, Guinea and Sierra Leone saw thousands of cases in large measles outbreaks that continued two or three years after the Ebola epidemic ended, Masresha says.
The international groups that fight measles worldwide, including the WHO, the CDC, the American Red Cross, the United Nations children’s charity UNICEF and the UN Foundation, are desperate to avoid a repeat. In part to spur countries into action, the WHO and the CDC have prepared risk assessments for countries plagued by recurrent measles epidemics, focusing on Africa.
Why measles deaths are surging — and coronavirus could make it worse
Ethiopia, Africa’s second-most populous country, needed no prodding, says Meseret Zelalem, director of maternal and child health and nutrition at Ethiopia’s Ministry of Health. Just 60% of children there have received their routine immunizations, and the last mass vaccination campaign for measles was conducted in 2017. Then the country delayed its April 2020 campaign. Projections suggested that thousands of children would die of measles in 2020 and 2021 if the country did not act. Although it wasn’t clear whether Ethiopia could conduct a campaign safely during a pandemic, Zelalem says, “We found a way.” In July last year, outfitted with almost 395,000 face masks, more than 340,000 bottles of hand sanitizer and new protocols to ensure physical distancing, vaccinators fanned out across the country, reaching 14.5 million children — more than 95% of the target population (M. Nigus et al. Pan Afr. Med. J. 37 (Suppl. 1), 36; 2020).
Ethiopia was the first large country to conduct a campaign in the current pandemic era, and international organizations hoped it would be a model for the rest of the world. Chad, a country that the CDC and WHO predicted was barrelling towards a huge outbreak, launched a measles campaign in January.
But other countries, worried about exacerbating the pandemic, still have their campaigns on hold. Masresha fears that Guinea, Gabon, Angola and Kenya will face major outbreaks if they don’t conduct campaigns by the middle of this year.
Now, as COVID-19 vaccines arrive in Africa, health workers are likely to concentrate on delivering those rather than measles vaccines. “We will see more and more delays because of COVID,” says Goodson. “We see over and over again that countries that delay campaigns have an outbreak.”
Polio setbacks
The three-decade-long drive to eradicate polio was going backwards even before COVID-19 hit, and the pandemic has made a bad situation worse. In 2019 and 2020, cases of wild poliovirus rose in Pakistan and Afghanistan, the last two countries where it is endemic. And although Africa is free of wild poliovirus, polio strains derived from vaccines are raging there: these emerge in rare instances when the live, weakened virus used in Albert Sabin’s oral polio vaccine mutates into a strain that can spread in under-immunized communities and regains its ability to paralyse.
Cases of paralysis caused by both wild and vaccine-derived strains are now higher than they have been in years (see ‘Polio: a long way from eradication’), rising to a combined 1,216 cases in 2020 from 554 in 2019, which in turn was higher than in 2018. (For every paralysis case, there can be 200 further infections.)
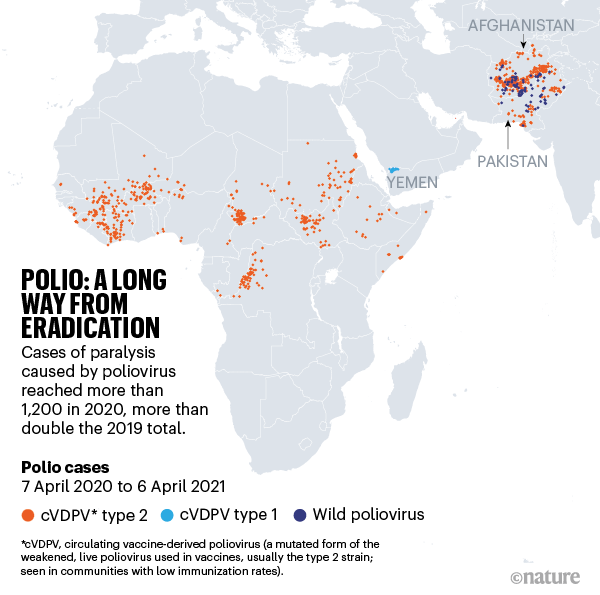
In March last year, the Global Polio Eradication Initiative (GPEI) in Geneva called for a pause in mass vaccination campaigns and repurposed some of its surveillance and laboratory infrastructure to the COVID-19 fight. More than 60 campaigns in 28 countries were postponed. Unpublished models from Imperial College London soon projected that polio cases could increase exponentially in some places if campaigns did not resume quickly. In late May, the GPEI called on governments to restart as soon as they had proper safeguards in place. But by the time they did so, the poliovirus, given free rein, had already taken off.
In Pakistan and Afghanistan, wild poliovirus expanded its reach, spreading from known reservoirs into previously polio-free areas — although total cases of paralysis in those two countries actually declined from 176 in 2019 to 140 in 2020. But there’s still a long way to go. In an eradication programme, says Aidan O’Leary, the head of the GPEI, “the only number that counts is zero”. At the same time, cases of paralysis caused by vaccine-derived poliovirus increased from 22 in 2019 to 135 last year in Pakistan, and the strain jumped the border into Afghanistan, causing paralysis in 308 children in 2020. A vaccine-derived virus from Pakistan is now paralysing children in Tajikistan, which last saw a large polio outbreak in 2010.
Africa declared free from wild polio — but vaccine-derived strains remain
In Africa, vaccine-derived strains spread easily without any response, says Pascal Mkanda, the WHO’s coordinator for polio eradication in Africa. Cases climbed from 328 in 2019 to more than 500 in 2020, as the virus hopscotched the continent, affecting 6 new countries to bring the total to 18. Help might come from a new vaccine against vaccine-derived strains, which was approved in November, but it has yet to prove its mettle in the real world.
It’s tough to tease apart exactly how much of the current spike was inevitable, given how widespread the virus was in 2019, but the pause “absolutely gave the opportunity for the virus to spread”, says Michel Zaffran, who retired as head of the GPEI in February.
Because vaccine-derived poliovirus is spreading so fast, stopping it is the first priority in Pakistan and Afghanistan while simultaneously hammering away at the wild virus, says Hamid Jafari, director of the polio eradication programme in the WHO’s eastern Mediterranean region. Massive campaigns are under way. In Africa, which has been plagued by slow, poor-quality campaigns that failed to reach enough children, the GPEI is now deploying rapid-response teams to act as soon as a vaccine-derived poliovirus is detected.
The GPEI must also deal with the problems that derailed the eradication effort before COVID-19. In Pakistan and Afghanistan, those include rumours about vaccine safety, vaccine refusals, the killing of polio workers, apathy and, in Afghanistan, a Taliban bar on polio vaccinations that has left some 3.3 million children out of reach. In Africa, the situation has been complicated by unfounded rumours that polio vaccinators are using African children as guinea pigs to test COVID-19 vaccines.
Still, both Jafari and Mkanda say campaigns have led to a drop in cases in the past few months; now the key is to prevent a resurgence in the upcoming peak season for polio transmission. “The complexity of COVID has not gone away, but we are in a very different situation than in July,” Jafari says. Still, many veterans of the polio eradication effort have abandoned their rosy predictions that polio will be defeated next year, which has been a constant refrain. Maybe in two or three years, says O’Leary.
For now, many countries remain laser-focused on COVID-19, with old problems such as measles, polio and TB taking the back seat. Other nations, such as Ethiopia and India, are already laying the groundwork for the long road back. Scientists and advocates talk optimistically about ‘building back better’, because deaths and illness from these old foes were too high before COVID-19. But with the course of the pandemic uncertain and the COVID-19 vaccine roll-out only just beginning, no one is talking about when that might happen.
Nature 592, 502-504 (2021)